Capsule Endoscopy
Capsule endoscopy is a procedure used to record internal images of the gastrointestinal tract for use in medical diagnosis. The capsule is similar in shape to a standard pharmaceutical capsule, although a little larger, and contains a tiny camera and an array of LEDs powered by a battery. After a patient swallows the capsule, it passes along the gastrointestinal tract taking a number of images per second which are transmitted wirelessly to an array of receivers connected to a portable recording device carried by the patient. The primary use of capsule endoscopy is to examine areas of the small intestine that cannot be seen by other types of endoscopy such as colonoscopy or esophagogastroduodenoscopy (EGD).
Dr Arti Rattan uses Capsule Endoscopy to find the cause of Gastrointestinal Bleeding which can lead to Iron Deficiency Anaemia, to diagnose IBD, to diagnose Celiac Disease and scan for polyps. Capsule endoscopy can also show tumors in the small intestine or other parts of the digestive tract.
Endoscopic ultrasound
Endoscopic ultrasound or echo-endoscopy is a minimally invasive medical procedure in which endoscopy is combined with ultrasound to obtain detailed images of the lining and walls of your digestive tract and chest, nearby organs such as the pancreas and liver, and lymph nodes. Dr Noureddin will use this procedure to evaluate cancer of the colon, oesophagus, pancreas or stomach, and Ampullary cancer, Lymphoma, Barrett’s Oesophagus, Neuroendocrine tumors, Pancreatitis and pancreatic cysts and Bile Duct Stones
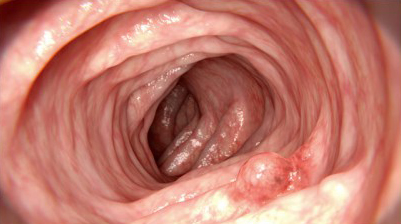
Endoscopic Mucosal Resection
Gastrointestinal endoscopic mucosal resection (EMR) is a procedure used to remove abnormal tissue, tumors and other precancerous growths from the lining of the digestive tract without surgery.
Endoscopic mucosal resection is performed using an endoscope, a long, narrow tube equipped with a light and video camera. During EMR of the upper digestive tract, the doctor passes the endoscope down your throat into your esophagus, stomach or upper part of the small intestine. For the colon and rectum, the doctor guides the tube up through the anus. Instruments are guided through this tube to remove growths or polyps. Because there is no incision, patients generally recover faster, with less pain than from regular surgery and can return home the same day.
EMR is usually done to treat a health condition. However, your doctor may also collect samples of tissue during the procedure. Examination of this tissue can help your doctor make a diagnosis. For example, if you have cancer, EMR can help determine if the cancer has spread to tissues beneath the digestive tract lining.
Disclaimer:
The information provided on this site is intended to educate the reader about certain medical conditions and certain possible treatment. It is not a substitute for examination, diagnosis, and medical care provided by a licensed and qualified health care professional. If you believe you, or someone you know suffers from the conditions described herein, please see your health care provider immediately. Do not attempt to treat yourself or anyone else without proper medical supervision.